What is perineural injection therapy (PIT)?
Certain patients with chronic pain are not candidates for joint replacement, PRP or stem cell therapies and other patients are non-responsive to conventional medicine solutions. Common problems such as trauma, arthritis, sports injury, overuse, occupational or surgical injuries can cause nerve injury may benefit from Perineural Injection Therapy (PIT).
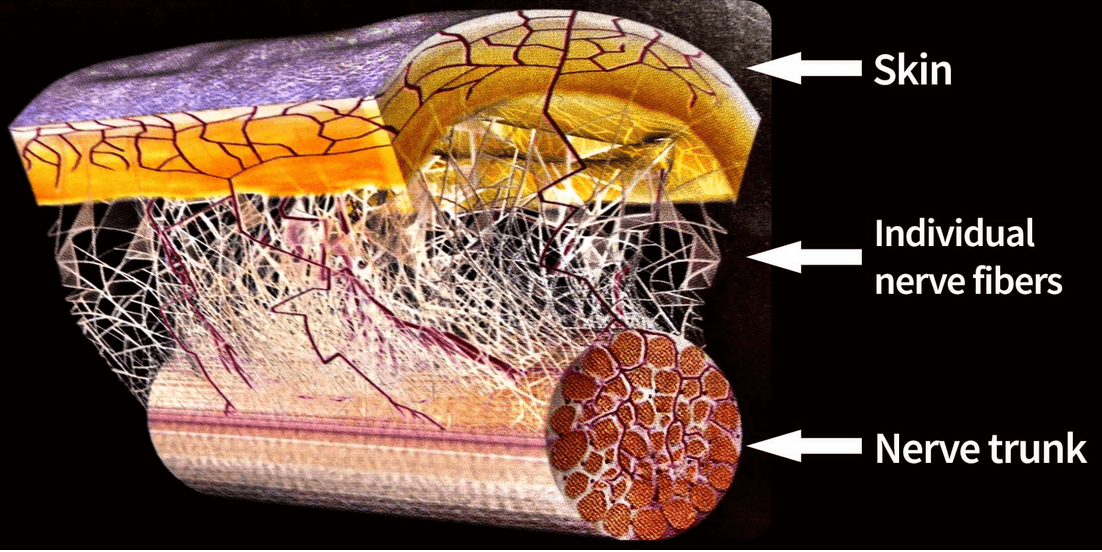
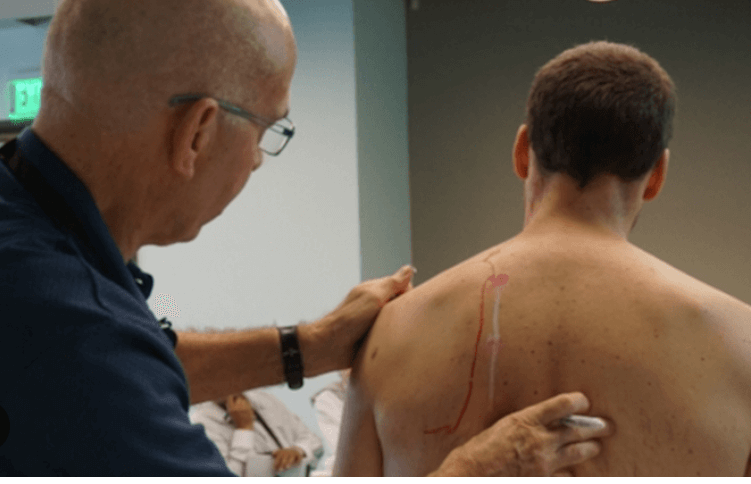
Perineural injection therapy (PIT), aka neural prolotherapy, is one of the latest advancements in regenerative medicine. It targets cutaneous nerves as a potential pain generator. Perineural Injection Therapy (PIT) targets neurogenic inflammation in subcutaneous nerves that potentially generates pain providing substantial pain control for neurogenic / neuropathic pain.
PIT therapies reduce target pain that is caused by inflamed or injured nerves which relay distressed cell signals to the brain resulting in persistent pain that may be unresponsive to pain medication. Secondary, injured nerves release a series of substances known as Nerve Growth Factor (NGF), substance P (P for pain) and calcitonin gene related peptide (CGRP) and others inhibiting the healing of affected muscles, tendons, and ligaments, resulting in chronic inflammation, sensitivity, and pain (neurogenic / neuropathic).
When injured or inflamed, nerve cells signal the brain by producing biological substances causing pain sensation and release out of the cell signaling the brain. The injured nerve continues to send a pain message to the brain even though the nerve is not being stimulated by pain. This creates a “short circuit” much like an open wire lying on the floor with electricity flowing through it. The substances that cause pain also prevent tissues such as muscles, tendons, and ligaments from healing. The term used to describe these inflamed nerves is called neurogenic inflammation.